The Centers for Medicare & Medicaid Services (CMS) has released the final instructions for the Calendar Year (CY) 2026 Part D Redesign Program, marking a significant milestone in the ongoing efforts to improve the Medicare Part D program. As a crucial component of the Medicare system, Part D provides prescription drug coverage to millions of beneficiaries across the United States. The final CY 2026 Part D Redesign Program instructions aim to enhance the program's efficiency, transparency, and beneficiary experience. In this article, we will delve into the key aspects of the final instructions and their implications for stakeholders.
Background and Objectives
The Part D Redesign Program is designed to address the evolving needs of Medicare beneficiaries, while also promoting competition, innovation, and affordability in the prescription drug market. The program's primary objectives include:
Improving the beneficiary experience through enhanced plan offerings and streamlined enrollment processes
Increasing transparency and accountability among Part D sponsors
Reducing costs and improving the overall value of prescription drug coverage
Key Provisions of the Final CY 2026 Part D Redesign Program Instructions
The final instructions outline several key provisions that will shape the future of the Part D program. Some of the notable changes include:
Enhanced Plan Flexibility: Part D sponsors will have greater flexibility to design plans that meet the unique needs of beneficiaries, including the ability to offer more targeted and specialized benefits.
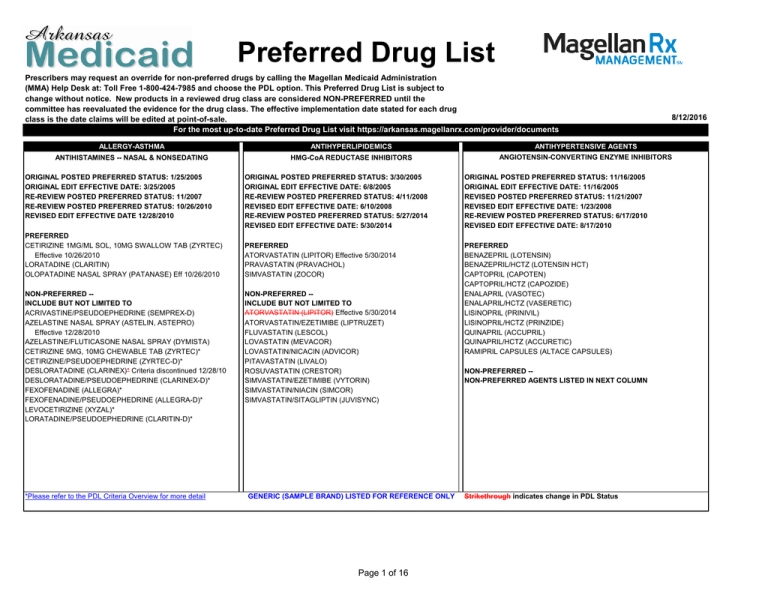
Increased Transparency: Sponsors will be required to provide more detailed information about their plans, including costs, coverage, and formulary details, to facilitate informed decision-making by beneficiaries.
Streamlined Enrollment Processes: The final instructions introduce new enrollment processes aimed at reducing beneficiary confusion and facilitating smoother transitions between plans.
Implications for Stakeholders
The final CY 2026 Part D Redesign Program instructions have significant implications for various stakeholders, including:
Part D Sponsors: Sponsors will need to adapt to the new program requirements, investing in plan design, transparency, and enrollment process enhancements to remain competitive.
Medicare Beneficiaries: Beneficiaries can expect improved plan options, increased transparency, and streamlined enrollment processes, ultimately leading to better prescription drug coverage and more informed decision-making.
Healthcare Providers: Providers will need to stay informed about the changes and their impact on patient care, ensuring that they can effectively navigate the evolving Part D landscape.
The final CY 2026 Part D Redesign Program instructions mark an important step forward in the evolution of the Medicare Part D program. By promoting competition, transparency, and innovation, these instructions have the potential to improve the beneficiary experience, reduce costs, and enhance the overall value of prescription drug coverage. As stakeholders navigate these changes, it is essential to stay informed and adapt to the new program requirements, ultimately ensuring that Medicare beneficiaries receive the best possible care and support.
By understanding the final CY 2026 Part D Redesign Program instructions, stakeholders can unlock the full potential of the Medicare Part D program, driving positive change and improved outcomes for millions of beneficiaries across the United States.
Word count: 500


+cropped.png?format=2500w)